Press Release
Johns Hopkins APL, Partners Earn NIH Neuromod Prize to Expand Spinal Cord Injury Research
The Johns Hopkins Applied Physics Laboratory (APL) in Laurel, Maryland, is among the institutions selected as Phase 1 winners for the Neuromod Prize, a $9.8 million initiative from the National Institutes of Health (NIH) Common Fund’s Stimulating Peripheral Activity to Relieve Conditions program. The competition is designed to accelerate the development of targeted neuromodulation therapies.
The project that received the award is a neuromodulation therapy for spinal cord injuries, commonly known as SCIs, and is being led by the University of Louisville’s Kentucky Spinal Cord Injury Research Center, in collaboration with the Kessler Foundation and Medtronic.
Neuromodulation has the potential to treat nearly any condition in the body through regulation of the nervous system. Recent innovations in device technology and an improved understanding of the interactions between the nervous system and target tissues and organs have led to a breakthrough moment in the field, according to the NIH. In January, the agency launched the Neuromod Prize to encourage scientists, engineers and clinicians to develop new therapies.
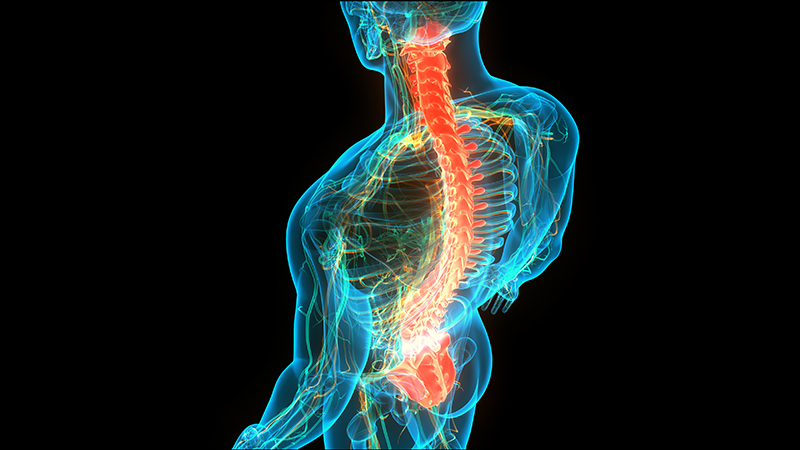
SCI interventions are still in their infancy compared with advances made for other types of injuries and diseases. These injuries are so complex that disruption of the autonomic nervous system occurs, potentially resulting in cardiovascular, respiratory and bladder dysfunction. These consequences hinder recovery and drastically diminish quality of life.
APL and its collaborators proposed StimXS, a novel communication and analysis system that integrates multimodal sensor information simultaneously to stabilize blood pressure and improve respiratory and bladder function in individuals living with SCIs.
StimXS builds on University of Louisville (UofL) research and is designed to enable the integration of biomarkers from external sensor data (bladder, cardiovascular and respiratory modules) as well as human-input data (a “human-in-the-loop” sensor module). The system will communicate with Medtronic’s implanted neurostimulator, which is under investigational use for the treatment of SCI, using customized applications and control systems.
“Voice recognition capabilities are specifically valuable for independent use in the home and community for those with limited arm and hand function associated with cervical SCIs,” explained Susan Harkema, a professor in UofL’s Department of Neurological Surgery, Anatomical Sciences and Neurobiology, and the associate director of the Kentucky Spinal Cord Injury Research Center. “More importantly, for this population, these advancements will also provide a hands-free approach when transitioning between various activities of daily living.”
The APL team brings extensive experience in software development for real-time system control, as well as artificial intelligence (AI) and machine-learning applications for image analysis, electrophysiology and noninvasive neuroimaging. APL will develop AI algorithms to monitor the sensor module data and inputs from the human-in-the-loop module and fine-tune the device’s neurostimulator programs.
“These algorithms will provide accuracy and precision by learning from historical and novel data sets, receiving continuous sensor data, and monitoring targeted performance parameters and biomarkers,” explained APL’s Francesco Tenore. “Additionally, an application called the Global Datacron will store all historical program configurations, along with targeted performance parameters and biomarkers, and make them accessible for all researchers and clinicians.”
APL and its collaborators received $100,000 and an exclusive invitation to participate in Phase 2 of the competition, which will involve Phase 1 winners building on their submissions by conducting proof-of-concept studies. From there, up to four winners may be selected to advance to Phase 3. The competition will also provide additional resources to help accelerate and develop proposed solutions.